Schizophrenia is a severe neuro-psychiatric disease that affects approximately 1% of the world's population. It is characterized by a wide variety of symptoms that include both positive symptoms (such as hallucinations and delusions) and negative symptoms (such as lack of emotion or motor control). While many factors have been associated with developing schizophrenia—including genetics, early environment, neurobiology, and psychological and social processes—the exact cause of the disease is unknown.
Causes of schizophrenia
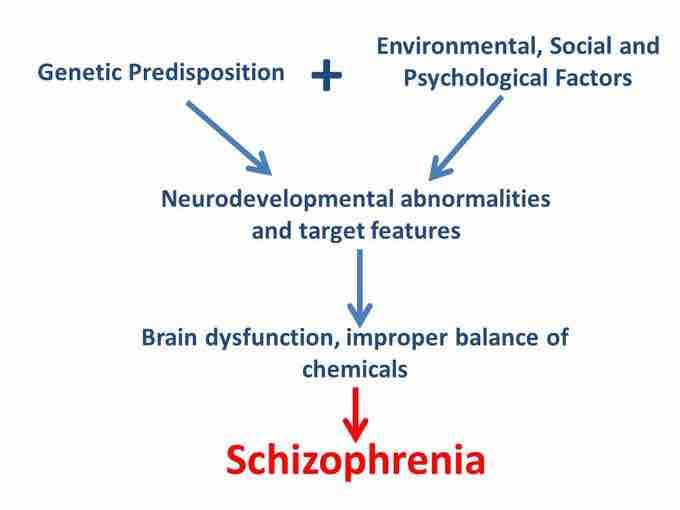
A variety of factors have been associated with schizophrenia, including genetic predisposition, environmental factors, and neurotransmitter imbalances.
Genetic Factors
With the advancement of scientific measures such as whole genome sequencing, researchers are able to better understand the genetic factors associated with schizophrenia. Scientists have discovered specific genes (such as VIPR2) and genetic mutations (including copy number variation, or CNV) that are directly related to the disease.
If an individual has a family member with schizophrenia, they are more at risk for developing the disorder than an individual without a family history of the disease. Concordance rates, or the frequency of an individual developing schizophrenia if a relative suffers from it, are remarkably high. Identical twins show a 50% concordance rate; individuals with two parents with the disease show a 40% rate; fraternal twins show a 12%–15% rate; individuals with one schizophrenic parent show a 12% rate; and individuals with a schizophrenic non-twin sibling show an 8% rate of also having the disease. In contrast to this, the general population has a 1% chance of developing the disease.
These rates indicate that the disorder is largely inherited, but they also suggest that additional factors influence the development of schizophrenia. It is generally thought that individuals can be predisposed to schizophrenia through genetic vulnerability, which is then triggered by environmental stimuli. Most researchers agree that both genetic vulnerability and environmental triggers must be present for the disease to develop.
Environmental Factors
While the exact environmental trigger(s) that influence the development of schizophrenia are unknown, scientists suspect that prenatal exposure to the flu or famine, obstetric complications, central-nervous-system infections in early childhood, and psychosocial stress in childhood and early adulthood may be linked to the disease.
Psychosocial environmental stressors can range from parental divorce to suffering from childhood abuse. Individuals who later develop schizophrenia may also be more socially anxious and have emotional fluctuations. It is unclear if these factors exacerbate stressors, are the result of these stressors, or stem from a third variable.
The pathenogenic theory of schizophrenia suggests that in-utero exposure to pathogens that affect the central nervous system may cause a predisposition for the development of schizophrenia.
It has been noted that people with schizophrenia often come from families with a low socioeconomic status. Some theorists suggest environmental stress associated with lower-class living may affect brain development, triggering the disease in genetically susceptible individuals. However, the correlation between socioeconomic status and schizophrenia could also be explained by the "downward drift" theory. This theory posits that because people with schizophrenia cannot hold a job or function well in society untreated, they "drift down" to a lower status.
While much research has been done regarding whether childhood experiences play a significant role in the development of schizophrenia, not much has been determined at this time.
Neurological Factors
Research has shown that neurotransmitter activity is significantly related to schizophrenia. The study of neurotransmitters and schizophrenia is particularly important because most of the pharmaceutical treatment options for the disease involve regulating these chemicals.
The Dopamine Theory of Schizophrenia
The dopamine hypothesis of schizophrenia is a model used by scientists to explain many schizophrenic symptoms. The model claims that a high fluctuation of levels of dopamine can be responsible for schizophrenic symptoms. The simplest version of this theory suggests that schizophrenia is associated with an increase of dopamine in the central nervous system.
Additional research has identified two dopamine pathways in particular that are associated with the positive and negative symptoms of schizophrenia. The first is the mesolimbic system, which affects areas regulating reward pathways and emotional processes; the second is the mesocortical system, which affects the prefrontal cortex, areas that regulate cognitive processing, and areas involved with motor control. Excess activity in the mesolimbic pathway and lack of activity in the mesocortical pathway are thought to be responsible for positive and negative symptoms, respectively.
The dopamine hypothesis has helped progress the development of antipsychotics, which are drugs that stabilize positive symptoms by blocking dopamine receptors. The fact that these medications have been shown to treat psychosis supports the dopamine theory.
Other Neurotransmitters
Dopamine is not the only neurotransmitter associated with schizophrenia, although it can be argued that it is the most studied. Seratonin and glutamate have also been linked with schizophrenia. Increased levels of seratonin are associated with positive symptoms. Glutamate has been theorized to exacerbate hyperactivity and hypoactivity in dopamine pathways, affecting both positive and negative symptoms.
Brain Areas Associated with Schizophrenia
In addition to neurotransmitters, specific neural circuitry in various areas of the brain has been linked to schizophrenia. Disregulation of neurotransmitters in the association cortex may explain why people with schizophrenia are not able to properly sort or filter information. The medial temporal lobe and hippocampus are associated with symptoms such as lack of focus and emotional regulation. The thalamus can also affect symptoms in various ways: a decrease in the size of the thalamus may lead to hallucinations, and a breakdown in one of the neural pathways within the thalamus is associated with disjointed associations. Finally, the basal ganglia also affect schizophrenia. This area is involved with the integration of information from cortical areas and may also influence disjointed perceptions of environmental information.