The accessory sex glands, including the seminal, prostate glands, and bulbourethral glands, produce seminal fluid and clean and lubricate the urethra.
Seminal Gland Anatomy
Each seminal gland forms as an outward growth of the wall of ampulla of each vas deferens. They are curled and folded within the gland and can spread out to approximately 5 cm, but the unfolded length is approximately 10 cm. The excretory duct of the seminal gland opens into the vas deferens as it enters the prostate gland.
Seminal Gland Physiology and Function
The seminal vesicles secrete a significant proportion of the fluid that ultimately becomes semen. Lipofuscin granules from dead epithelial cells give the secretion its yellowish color. About 50 - 70% of seminal fluid in humans originates from the seminal vesicles, but is not expelled in the first ejaculate fractions which are dominated by spermatozoa and zinc-rich prostatic fluid. Seminal vesicle fluid is alkaline, resulting in human semen with a mildly alkaline pH. This helps neutralize the acidity of the vaginal tract, prolonging the lifespan of sperm. Acidic ejaculate (pH <7.2) may be associated with ejaculatory duct obstruction. The vesicle produces a substance that causes the semen to become sticky after ejaculation, thought to help keep the semen near the cervix.
The thick seminal vesicle secretions contain proteins (including enzymes), mucus, fructose, vitamin C, flavins, phosphorylcholine, and prostaglandins. The high fructose concentrations provide nutrient energy for the spermatozoa when stored in semen in the laboratory. Spermatozoa ejaculated into the vagina are not likely to have contact with seminal vesicular fluid, but transfer directly from the prostatic fluid into the cervical mucus as the first step on their travel through the female reproductive system.
Seminal vesicle fluid is expelled under sympathetic contraction of the muscularis muscle coat. In vitro studies have shown that sperm expelled together with seminal vesicular fluid show poor motility and survival and less-protected chromatin. Thus, the exact physiological importance of seminal vesicular fluid is unclear. It may be a developmental rest, such as in some rodents where the last part of the ejaculate forms a spermicidal plug to reduce the chances for sperm from a later-arriving male to proceed to the oocyte.
Prostate Gland Anatomy
The prostate surrounds the urethra just below the urinary bladder and can be felt during a rectal exam. It is the only exocrine organ located in the midline in humans and similar animals. Within the prostate, the urethra coming from the bladder is called the prostatic urethra and merges with the two ejaculatory ducts. The prostate is sheathed in the muscles of the pelvic floor, which contract during the ejaculatory process.
Prostate Gland Physiology and Function
The prostate secretes a slightly acidic fluid, milky or white in appearance, that usually constitutes 20–30% of the volume of the semen along with spermatozoa and seminal vesicle fluid. The prostatic fluid is expelled in the first ejaculate fractions, together with most of the spermatozoa. In comparison with the few spermatozoa expelled in seminal vesicular fluid, those expelled in prostatic fluid have better motility, longer survival, and better protection of the genetic material. The prostate also contains some smooth muscles that help expel semen during ejaculation.
To work properly, the prostate needs male hormones (e.g., testosterone), which are produced mainly by the testes. Some male hormones are produced in small amounts by the adrenal glands. However, dihydrotestosterone regulates the prostate. A healthy human prostate is slightly larger than a walnut in adult males, with a weight ranging between 7 and 16 grams.
Bulbourethral Glands
Bulbourethral glands are located posterior and lateral to the membranous portion of the urethra at the base of the penis, between the two layers of the fascia of the urogenital diaphragm in the deep perineal pouch. They are enclosed by transverse fibers of the sphincter urethrae membranacea muscle. The bulbourethral glands are compound tubulo-alveolar glands, each approximately the size of a pea. They are composed of several lobules held together by a fibrous covering. Each lobule opens into a duct that joins with the ducts of other lobules to form a single excretory duct. This duct is approximately 2.5 cm long and opens into the urethra at the base of the penis. The glands gradually diminish in size with advancing age.
During sexual arousal, each gland produces a clear, salty, viscous secretion known as pre-ejaculate. This fluid helps to lubricate the urethra for spermatozoa to pass through, neutralizes traces of acidic urine in the urethra, and helps flush out any residual urine or foreign matter. It is possible for this fluid to pick up sperm remaining in the urethral bulb from previous ejaculations and carry them out prior to the next ejaculation.
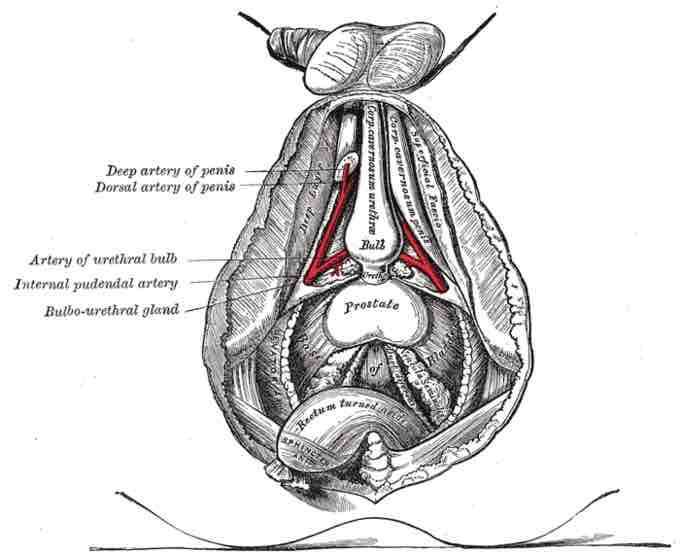
Bulbourethral Gland
Image shows internal view of penis and male sexual anatomy. The bulbourethral gland is labeled at center left.
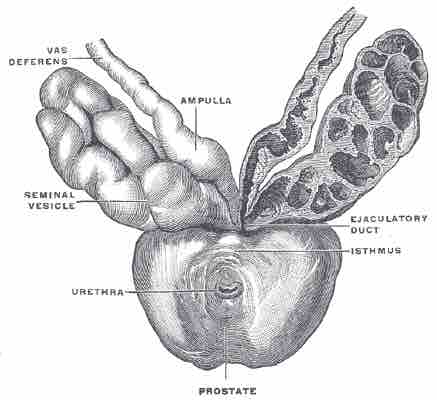
Prostate
Prostate with seminal vesicles and seminal ducts, viewed from the front and above, including the urethra, seminal vesicle, vas deferens, ampulla, ejaculatory duct, and isthmus.